Pharmacy and prescription drugs
Your pharmacy benefit is the part of your health insurance that covers drugs and medications that are prescribed by doctors in your plan’s network. The medications covered are generally ones that you get from a pharmacy, not the ones a doctor gives you in the office or a hospital (those are covered under your medical benefits).
Do I have pharmacy benefits?
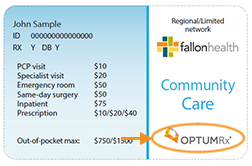 Whether or not you have pharmacy benefits through Fallon Health depends on the plan you're enrolled in and/or the employer group you get your insurance through. The simplest way to check if you have pharmacy benefits is to look at your health plan ID card. If you have pharmacy benefits through Fallon, you'll see an OptumRx logo on the front of your card. You can also check your Summary of Benefits, Evidence of Coverage or other plan documents for details about your pharmacy benefits and drug coverage.
Whether or not you have pharmacy benefits through Fallon Health depends on the plan you're enrolled in and/or the employer group you get your insurance through. The simplest way to check if you have pharmacy benefits is to look at your health plan ID card. If you have pharmacy benefits through Fallon, you'll see an OptumRx logo on the front of your card. You can also check your Summary of Benefits, Evidence of Coverage or other plan documents for details about your pharmacy benefits and drug coverage.
How does my pharmacy benefit work? What will my costs be?
Formulary
Fallon plans that include pharmacy benefits have a formulary, which is a list of drugs that the plan covers. A formulary is sometimes called a covered drug list. Most of the time, you can’t get coverage for drugs that are not on the list.
Tiers
A plan's formulary or covered drug list is usually organized into tiers, each with a different copayment or coinsurance level. A common setup is to have four tiers.
In a typical three-tier formulary:
- Tier 1 contains lower-cost generic drugs, which have the same active ingredients and effects as brand-name drugs. With the lowest copayments, this tier gives you greater savings for many medications you commonly use.
- Tier 2 contains preferred brand-name drugs.
- Tier 3 contains non-preferred brand-name drugs.
Cost-share, copayments, coinsurance and deductibles
Depending on the plan you're enrolled in, you may share part of the cost with your insurance for each prescription.
- A copayment is a set dollar amount that you pay for each prescription
- Coinsurance is when you pay a percentage of the drug’s price.
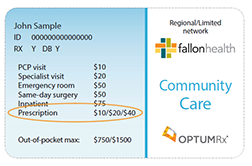 Your copayment is determined by the drug’s tier on the covered drug list. For example, you might have a $10 copayment for a Tier 1 drug, but pay $20 for one on Tier 2 or $40 for one on Tier 3—still significantly less than paying the full retail price. If your plan has coinsurance instead, you’ll pay a percentage of the drug’s cost, regardless of the tier it’s on. If you have a deductible, you may have to satisfy the deductible before a drug will be covered.
Your copayment is determined by the drug’s tier on the covered drug list. For example, you might have a $10 copayment for a Tier 1 drug, but pay $20 for one on Tier 2 or $40 for one on Tier 3—still significantly less than paying the full retail price. If your plan has coinsurance instead, you’ll pay a percentage of the drug’s cost, regardless of the tier it’s on. If you have a deductible, you may have to satisfy the deductible before a drug will be covered.
Check your Summary of Benefits, Evidence of Coverage or other plan documents for details. Depending on which plan you're enrolled in, your health ID card may also show your copayments or coinsurance for each tier.
How do I find out if a drug is covered?
You can find out if your plan covers a drug by checking the printed covered drug list that you may have received with your plan materials. You can also search for the drug on our online drug formulary.
Search the online drug formulary ⇒
Generic alternatives
Generic drugs can help you save money on your out-of-pocket drug costs. Generic medications contain the same ingredients in the same amount and the same form as their brand-name counterparts. They are just as safe and work just as well—but they usually cost much less. With most plans, your prescription will automatically be filled with a generic drug, if one is available. This saves you and the health plan money. But, if your doctor wants to make sure you take a brand-name drug, he or she can specify that on the prescription
Plus, all the generic drugs on the covered drug list have been reviewed by both the FDA and the health plan's Pharmacy and Therapeutics Committee, so you can be confident that they are safe and effective.
Drugs that need prior authorization
Sometimes, a drug requires prior authorization. That means that your doctor must ask the health plan to cover the drug and provide medical information to back up the request before the drug will be covered. This “double-checking” step helps ensure the drug is being used safely and appropriately. A new drug without a track record of safety may require prior authorization, while an older drug that’s been proven safe and effective would not.
Your doctor can submit prior authorizations online through an electronic prior authorization tool, or he or she can fax or call in the prior authorization. Your doctor can find information about prior authorizations in the Providers section of our website. You may want to check with your doctor or your pharmacy to make sure all necessary information was submitted before you pick up a prescription that requires prior authorization.
Drugs that require prior authorization are tagged as "PA" in our printed covered drug lists and in the online drug formulary.
Special instructions for certain drugs
Some drugs on our covered drug lists have limits or special instructions associated with them. Drugs that have limits or special instructions are tagged in our printed covered drug lists and in the online drug formulary.
Quantity Limits
A plan may limit the amount of a drug that can be dispensed at once, or limit the amount of time it can be taken. This helps prevent waste, overuse, misuse or potential harm.
If a drug has a quantity limit, you'll see a note in the "Limit" column in our printed covered drug lists and in the online drug formulary.
Step Therapy
Some drugs are prescribed as part of step therapy. Step therapy is a process that starts with drugs that have been on the market for a longer period of time and have a proven track record rather than newer and more costly drugs. If your condition doesn't respond at first, a different drug is tried in sequence. Step therapy also helps ensure that you pay the least possible out-of-pocket expense for an effective medication for your condition.
Step therapy drugs will be marked with "ST" in our printed covered drug lists and in the online drug formulary.
Drugs that are new to the market
If the drug has been on the market for less than six months, then it may fall under a new-to-market policy. Such policies give medical experts time to review the data and approve clinical criteria for using it properly. Only then will the new drug go on the covered drug list.
Medications for chronic conditions
View our current list of medications for chronic conditions and applicable cost-sharing.
Where can I get my prescription medications filled?
Retail pharmacies
You can get your prescriptions filled at any pharmacy in your network. You generally won’t be covered for drugs from an out-of-network pharmacy.
Find a pharmacy in your network ⇒
Mail-order
You can also use our mail-order pharmacy which offers four ways to order prescriptions. In some cases, using the mail-order pharmacy can save you money. For instance, Fallon members can get up to a 90-day supply of Tier 1 and Tier 2 drugs for the cost of only two copayments.
Learn more about mail-order pharmacy ⇒
Specialty drugs
Some drugs, like infused or injectable drugs can only be ordered through the CVS Caremark Specialty Mail Order service.
Learn more about specialty drugs ⇒
More information to understand and use your pharmacy benefit
You can also determine your financial responsibility for a drug, order a refill for an existing unexpired mail-order prescription, find a location of an in-network pharmacy, conduct a pharmacy search based on zip code, determine potential drug-to drug-interactions, determine a drug’s common side effects and significant risks, and determine the availability of generic substitutes online on the OptumRx website.
Questions?
If you need help with your pharmacy benefits or formulary/covered drug list, please call our Customer Service Department at 1-800-868-5200 (TRS 711), Monday, Tuesday, Thursday, and Friday from 8 a.m. to 6 p.m. and Wednesday from 9 a.m. to 6 p.m. MassHealth members can call Fallon Customer Service at: 1-800-341-4848 (TRS 711) Monday through Friday, 8 a.m. to 6 p.m.