Pharmacy prior authorizations
Prior authorization process - all plans
Fallon Health collaborates with OptumRx (Fallon's Pharmacy Benefit Manager) and Prime Therapeutics Management (Prime) LLC to implement our prior authorization process. For all lines of business, OptumRx reviews pharmacy benefit drugs (patient self-administered drugs, including oral medications and Commercial/Medicaid member diabetic testing supplies). For Medicare members only, Fallon Health reviews glucose monitor and test strip requests. Prime reviews medical benefit drugs (physician-administered drugs, including home infusion).
How to locate criteria and PA forms - commercial, Medicare, NaviCare, and PACE plans
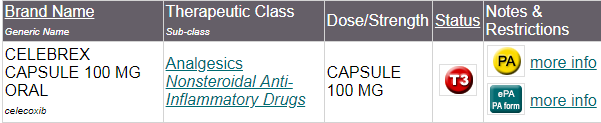
Please use the Online Formulary to determine which medications require Utilization Management (UM). Each drug with UM includes a link to the criteria, ePA, and fax form.
Example:
Important Information regarding the Massachusetts Standard PA Form and Commercial plan members
Please review the criteria posted on the Online Formulary prior to completing the PA form or submitting an ePA and provide all relevant data for each part of the criteria. If there is no specific field for the data on the PA form, please use the "Additional information pertinent to this request" field. For Commercial member PA requests, you must use the state-mandated standard PA form, or otherwise use ePA or telephone.
How to locate criteria and PA forms – Medicaid/MassHealth ACO plans
Please visit MassHealth’s website directly for online formulary listing, prior authorization criteria, and forms.
Prior authorizations MUST be submitted as indicated below.
Patient-administered drugs (pharmacy benefit) - all plans
2025 Update: Medicare glucose monitors and related testing supplies (including test strips and CGMs) for Medicare, NaviCare, and PACE plans are now reviewed by our partner, OptumRx. Please use the contact information below to submit these PA requests.
Our process offers you two ways to submit a prior authorization request for patient self-administered drugs:
- Electronic prior authorization tool (ePA)
- Call or fax
Electronic prior authorization tool (ePA)
Fallon and OptumRx have made submitting PAs easy, quick, and convenient. ePA is a secure and easy method for submitting, managing, tracking PAs, step therapy and non-formulary exception requests. It enables a faster turnaround time of coverage determinations for most PA types and reasons.
Using ePA, you can:
- Request clinical questions through your integrated EHR or the ePA website.
- Answer patient-specific clinical questions electronically and submit for review.
For more information about OptumRx prior authorizations:
Call or fax
To serve you quickly and efficiently, we have separate phone and fax numbers for our Medicare, Medicaid and commercial plans. To determine which phone or fax number to use, find the member's plan name on their ID card and locate it in the chart below.
When faxing, please use the form in the drug link on the Online Drug Formulary or, for Medicaid/MassHealth ACO plans, use the form on the MassHealth website.
|
Line of business
|
Phone
|
Fax
|
Mail
|
|
Commercial plans
|
1-844-720-0035
|
1-844-403-1029
|
Optum Prior
Authorization Department
P.O. Box 2975
Mission, KS 66201
|
|
Medicaid/MassHealth ACO
- Fallon 365 Care
- Berkshire Fallon Health
Collaborative
- Fallon Health-Atrius Health
Care Collaborative
|
1-844-720-0033
|
1-844-403-1029
|
Optum Prior
Authorization Department
P.O. Box 2975
Mission, KS 66201
|
|
Medicare
- Fallon Medicare Plus
- NaviCare
|
1-844-657-0494
|
1-844-403-1028
|
Optum Prior
Authorization Department
P.O. Box 2975
Mission, KS 66201
|
|
PACE
Summit ElderCare
|
1-844-657-0494
|
1-844-403-1028
|
Optum Prior
Authorization Department P.O. Box 2975
Mission, KS 66201
|
|
Fallon Health Weinberg-PACE
|
1-844-722-1701
|
1-844-403-1028
|
Physician-administered drugs (medical benefit) - all plans
Our process offers you two ways to submit a prior authorization request for physician-administered drugs:
- Electronic prior authorization web portal
- Call or fax
Electronic prior authorization web portal
Fallon and Prime have made submitting PAs easy, quick, and convenient through the Prime provider portal, gatewaypa.com. Please click "New Provider Access Request" under the "Sign In" box to request access.
Call or fax
- Call: 1-800-424-1740
- Fax: 1-888-656-6671
Plan member privacy is important to us. Our employees are trained regarding the appropriate way to handle members’ private health information.